Hands up who understands what osteoporosis is?
And why is a GP with self-confessed passion for women’s health talking about bones? Because, almost exclusively, this is an issue that affects women.
First, a few myths to be dispelled: Osteoporosis is not the same as osteoarthritis – two completely different animals. Osteoporosis in itself does not cause pain, there are no symptoms….until a bone snaps.
What is osteoporosis?
Osteoporosis is defined as a skeletal disorder characterised by compromised bone strength predisposing a person to an increased risk of fracture. In layman’s English: the intrinsic strength of bone becomes so low that even minor impact will result in fracture. The bones most commonly affected are neck of femur, the bone in the thigh, resulting in a hip fracture, and vertebrae. A vertebra is the name given to the individual back bones, stacked up like lego bricks, one on the other, encasing our spinal cord.
While a weak neck of femur bone will snap as a result of a fall; osteoporotic vertebrae often spontaneously collapse, causing tremendous pain, loss of height and that familiar hunched-over posture seen in elderly called kyphosis. Fracture of neck of femur is treated with a total hip replacement but there is not a lot that can be done for osteoporotic collapse vertebral fractures.
Osteoporotic fractures: the gory facts
Worldwide, osteoporosis causes more than 8.9 million fractures annually: an osteoporotic fracture every three seconds. One in three women over the age of 50 will experience an osteoporotic fracture. A prior fracture is associated with an 86 per cent increased risk of having another fracture. After a hip fracture, 10 to 20 per cent of patients, who were previously living interdependently, require long-term nursing care. Forty per cent of patients are unable to walk independently after a hip fracture. The mortality or likelihood of dying in the year after a hip fracture is 20-25 per cent: That’s a one in four chance of dying in the year after a hip fracture.
Contrasting that with breast cancer, compare the one in three risk of having an osteoporotic fracture in women over 50 with the one in 50 risk of getting breast cancer. When breast cancer is diagnosed localised in the breast, the likelihood of surviving five years after treatment is 99 per cent and 10 years is close to 80 per cent. In other words only one per cent of women over the age of 50 will die in the year after breast cancer diagnosis versus 20 per cent after a hip fracture.
Hopefully by now I have your attention. So what can we do?
What is bone?
What a lot of people do not realise is that bone is a dynamic organ, with bone constantly being laid down, then taken away or resorbed in a fluid cycle throughout our lives.
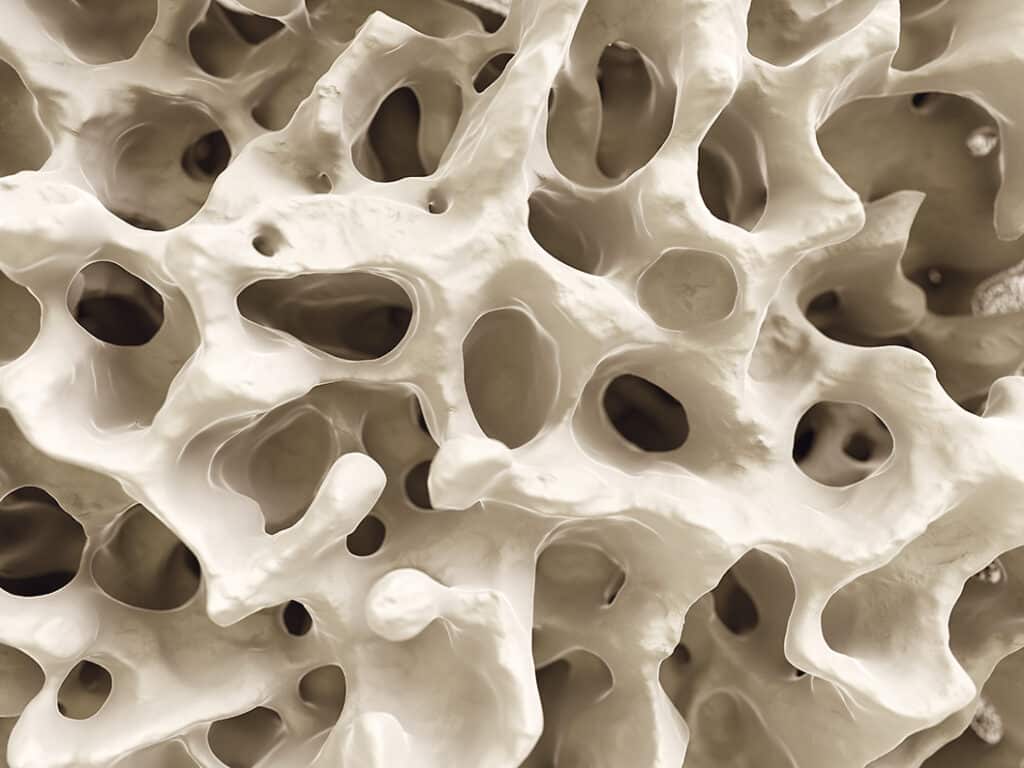
What makes bones strong is the combination of the bone density and quality. Bone is not a solid brick-like structure but looks a bit like honeycomb. So what we need is for that honeycomb structure to be as dense as possible, with few air spaces, plus we need the links in the honeycomb structure to be thick and strong.
Studies have shown that women naturally begin to lose bone strength from the age of 30. That cycle of bone being laid down / resorbed begins to tilt more towards resorption after 30 and then tips right over at menopause. Oestrogen supports bone build-up, therefore lack of oestrogen after menopause causes more rapid bone resorption, resulting in sharp drop-off in bone strength.
Risk factors
• Hereditary: osteoporosis does run in families. If you have a female family member who suffered a hip fracture under the age of 65 years, you need to see your GP for a risk assessment.
• Smoking and Low BMI, being very underweight, predisposes you.
• Nutrition: diets low in calcium and vitamin D.
• Alcohol: more than three units of alcohol per day: a large glass of wine is four units, ladies.
• Certain medical conditions: hypothyroidism, rheumatoid arthritis, some bowel diseases.
• Certain medications, in particular oral steroids.
• Inactivity – not just current but life-long is a significant risk.
• Previous fracture: As a health care professional, if I have a patient, especially female, who breaks an arm or leg bone after minor impact injury such as falling over on a pavement, I should be asking: was this an osteoporotic fracture?
• Amenorrhoea; the medical term for absence of menstrual periods might occur in conditions such as anorexia where extremely poor nutrition switches off ovulation and menstruation, putting that young woman into a low oestrogen state, resulting in bone resorption, not build-up.
The International Osteoporosis Foundation is a really useful source of information and assessment tools:
www.osteoporosis.foundation/patients
How de we prevent
osteoporotic fractures?
On two fronts: optimise bone build-up and minimise resorption.
Optimising bone strength starts in childhood. Weight bearing exercise, anything that involves walking or running stimulates bone strength. Exercise needs to continue from childhood into teens and through the 20s. A diet high in calcium and vitamin D.
Avoid excess alcohol and smoking, as much as is reasonable, in our youth.
Then, over the age of 30 to continue to build bone strength, we need regular weight bearing exercise, 30 minutes five times per week, plus a diet high in calcium and vitamin D.
Calcium and vitamin D – how much is enough?
Over the age of 50, a woman needs 1200mg of elemental calcium plus minimum 1000 I.U Vitamin D per day. There are a lot of ‘menopause vitamins’ out there but there is no evidence of benefit for bones or for menopause symptoms for any vitamins other than calcium and vitamin D. Most calcium tablets are in a salt form, often only 40 per cent of it being bioavailable.
As with all vitamins, the best way of taking calcium is in food. The International Osteoporosis Foundation has a useful daily calcium intake calculator.
When it comes to Vitamin D, we are basically living in the wrong country, as over 90 per cent of our vitamin D is generated as a result of sunshine reacting with our skin. Therefore everyone, not just women over 50, should take at least 1000 I.U vitamin D per day from September to April. Vitamin D is cheap to buy over the counter and easy to take. A high dose can just be taken once a week if you forget to take daily whereas calcium intake should be daily.
What about DEXA scans?
You will notice that I have not yet mentioned DEXA or bone strength scans. DEXA scans measure bone mass not bone quality. Results come back as normal, osteopaenia, or osteoporosis. For further explanation see: www.irishosteoporosis.ie.
However, the majority of osteoporotic fractures over the age of 50 occur in patients with osteopaenia, not osteoporosis. A DEXA by itself does not accurately tell you your risk of having an osteoporotic fracture over the next ten years. What DOES reliably calculate that is the FRAX risk assessment tool (frax.shef.ac.uk/)
You can do this yourself at home. International guidelines advise that if your 10-year hip fracture risk is greater than three per cent or your overall fracture risk greater than 20 per cent, you should have treatment.
The decision about whether you need to start treatment to prevent a fracture needs to be made following a consultation with your GP.
Treatment
Hormone replacement therapy, HRT, is licensed to treat, as well as prevent osteoporosis. It has been shown that being on HRT for four to five years between the ages of 50 and 60 years will halve the risk of osteoporotic hip fracture by the age of 65 years. There is no alternative non-hormonal remedy that has been shown to do this. HRT is licensed to both prevent and treat osteoporosis. If my patient chooses not to use HRT, that is entirely her decision, but my job is to make her aware of the long-term benefits, in particular for her bones.
Where HRT is contraindicated, such as after breast cancer, or if a woman does not wish to take HRT, medications called bisphosphonates taken in tablet form once a week, effectively treat osteoporosis. Both HRT and bisphosphonates can be initiated by your GP.
When a patient with osteoporosis is on treatment, either HRT or a bisphosphonate, we repeat the DEXA in one to two years, depending on the severity of the osteoporosis on baseline DEXA. It is possible to be on HRT and a bisphosphonate at the same time. Where the repeat DEXA does not show an improvement in bone strength, your GP should consider referral to an osteoporosis specialist called a rheumatologist.
Falls prevention equals
fracture prevention
For our elderly relatives – no loose rugs, support bars in the bathroom, well-fitting shoes and not slippers about the house, check eyesight with annual eye tests. Nutrition is very important. The loss of muscle mass called sacropaenia, which occurs with ageing, can be reversed with a high protein diet and even chair-based exercises if they are unable to get out for a walk every day.
All female readers need to be as worried about their bone health as they are about breast cancer. In short, ladies, we are far more likely to suffer a hip fracture than get breast cancer and, if we have a hip fracture over the age of 50, one in five of us will not make it through to the following Christmas.
What we are talking about here is primary prevention. To do that every woman at age 50 needs a consultation with their GP to have a holistic health check, looking at overall cardiovascular health and risks for same, bone health, as well as having that discussion about menopause, even if she has not been thinking about taking HRT. This is a bit of an alien concept in Ireland because most patients only go to their GP when they are unwell.
I have to add that this would become possible if the HSE paid for such a health check to be done by GPs, both for men and women.
Dr Stanley welcomes emails from readers requesting women’s health topics for future articles or links to information. Email drstanley@westcorkpeople.ie. We must emphasise that this is not a platform for medical advice.
Phone the clinic on 028 23456 to book an appointment with Dr Stanley.



