In almost 30 years of seeing women of all ages – in the UK for 29 years and here in Ireland for the past five months – female urinary symptoms are something that women rarely volunteer: I have to specifically ask about leaking or peeing problems.
What I find horrific is that women seem to resign themselves to peeing 20 times a day, wetting themselves, and assume this is another cross to bear for being a woman and getting older.
It is time to drag the ‘Ugly Duckling’ that is ‘Female Urinary Issues’ kicking and screaming and leaking…out of the dark cupboard under the stairs.
If I had my way, the HSE would run a public health campaign television advertisement that would go something like:
‘A choral line of women, 25 to 85 years, on a stage in a Moulin Rouge-style setting. The song is sung to the tune of Beyoncé’s ‘All the Single Ladies’, the women are belting out: ‘…to all the leaky ladies, all the leaky ladies!…” High kicks not possible for obvious reasons….and the choral line keeps splitting as ladies need to dash off to the porta-loos onstage in the background. Stage prop building labelled ‘Female Health Clinic’ descends from the rafters, encases the choral line…silhouettes of women being examined, issued medicines, then it rises again and all the ladies start high kicking and doing jumping jacks. END SCENE.
But it is not just about leaking. There are many different types of urinary symptoms that women are equally loath to discuss. A woman can suffer maddening urinary frequency often needing to pee 20-plus times a day; constantly worried about being able to find a toilet, she is reluctant to leave the house, restricts her fluids, takes less exercise and basically has her life ruled by her bladder.
Some women will also be up several times at night to pee, which means their sleep is poor and they are exhausted. Women can get recurrent cystitis, the lay-term for burning or discomfort passing urine. While some of these women are also dealing with other menopause symptoms, urinary symptoms in the under 45-year-olds is a commonly neglected area.
In terms of public health campaigns/public awareness of female urinary issues, since moving back here in March this year, all I have seen are ads for continence pads and pants – being advertised by very young-looking women. This horrifies me, as many urinary symptoms can be treated effectively: the ads should be saying go see your GP, not put a nappy on!
Where to start:
If you are having any urinary symptoms, go see your GP.
What your GP needs to do is take a detailed female health and urinary history. With pressure of work on female GPs in West Cork, I fear that it might not possible in a busy clinic, which often involves seeing 15 to 20 patients in a morning, to have time to undertake a detailed assessment. More than that, I have learned that many women find getting access to a female GP nigh on impossible. In addition, embarrassment often stops a woman coming to her GP, even when she can access a female GP. This was one of the many reasons I set up the dedicated Women’s Health Service in West Cork.
The following symptoms need to be specifically asked about:
Day time frequency: How many times per day do you need to pee? If there is a lot of frequency it is important to find out how much fluids, in particular caffeine drinks like tea or coffee, a woman drinks in a day.
Nocturia: How many times at night do you wake because you need to get up and pee?
Dysuria: Is there any discomfort, be it true burning or an uncomfortable feeling in the genital area, or perhaps low down on the front of the abdomen, over the bladder when you pass urine?
Urgency: This is defined as an urgent or sudden, dire urge to pee, often associated with discomfort.
Haematuria: Have you ever noticed blood in the pee when you are not on or near a period? Or ever noticed your urine looking a little pink in colour?
Incontinence: Is there any leaking? And if so what are the circumstances?
Is it when you laugh or sneeze, resulting in a very small amount of urine coming away? This is called Stress Incontinence.
If you have a full bladder or when you feel the urge to pee, are you able to hold on for a bit or do you need to go find a toilet NOW! Have you ever had a situation when you could not get to a toilet fast enough and completely emptied your bladder as a result? This is called Urge Incontinence.
Double micturition: When you have a pee, does it feel like you have not completely emptied your bladder? Do you get dripping or dribbling when you go to stand up when you thought you had finished?
Vulval / vaginal symptoms: Is there any associated dryness/soreness inside the vagina or of the skin of the external genital area? Is there a new or change to vaginal discharge? Is there a new man in the woman’s life? Sexually transmitted infections like Chlamydia can present with cystitis.
Abdominal bloating or swelling? Pelvic or intra-abdominal masses can rarely present with bladder symptoms.
Prolapse:Do you ever notice a feeling of something coming down in the vagina or a pressure feeling there?
Female health history:
How many children have you had? Pregnancy and vaginal delivery will weaken the pelvic floor, more so if any of the babies were very large, over 9lb, or if the delivery was associated with a major tear.
UTIs: Have you ever had urinary tract infections, UTIs, in particular recurrent infections?
Have you had any gynaecological surgery hysterectomy or repair of a prolapse?
Last period? Are you pregnant? Menopausal?
Medications: Is the woman on any medications that might cause urinary symptoms, like a diuretic. Other causes: has there been weight loss? Might this represent new onset diabetes?
So you begin to get the idea: female urinary symptoms can be many, varied and often multifactorial.
Examination:
You cannot fully evaluate a female patient with urinary symptoms without physical examination.
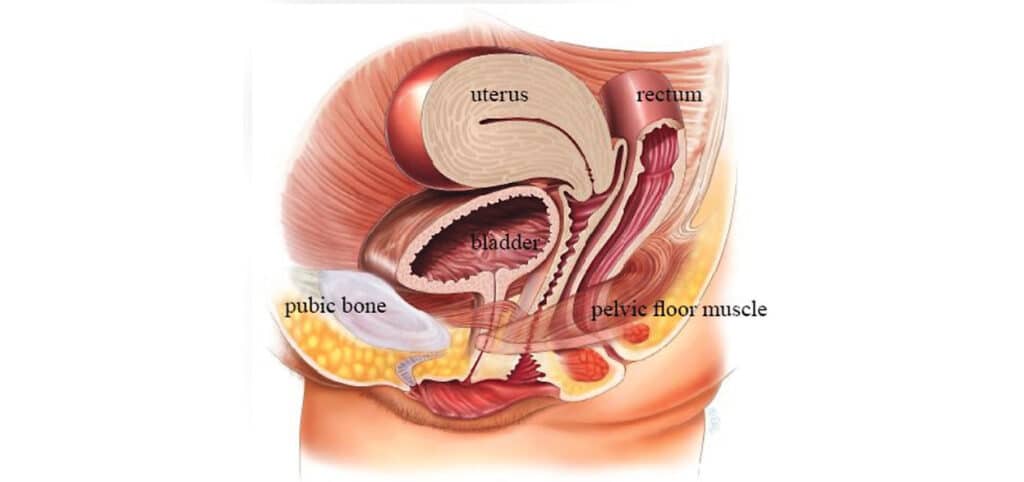
I will examine the external genital area, the vagina, assessing the pelvic floor strength, looking for any prolapse, assess for signs of pelvic or abdominal masses that might be pressing on the bladder.
In patients over 50, I look for signs of atrophic vaginitis or changes to the vagina and external genital area caused by lack of oestrogen.
Dipstick the urine – to rule out infection and check for blood in the urine.
Further investigation may be warranted. If there have been recurrent UTIs, a lot of frequency, any stress incontinence, I request a pelvic and bladder scan looking as to how the bladder is filling and emptying.
What next?
Next month – the causes of
female urinary symptoms and their treatment.



